- About
- SERVIZI
- INDUSTRIES
- Scienza e
Salute - Fashion & Retail
- Nature &
Agriculture - Manufacturing & Logistics
- Hotellerie &
Real Estate - Bellezza, Sport e
Benessere
- Scienza e
- News
- CONTATTI
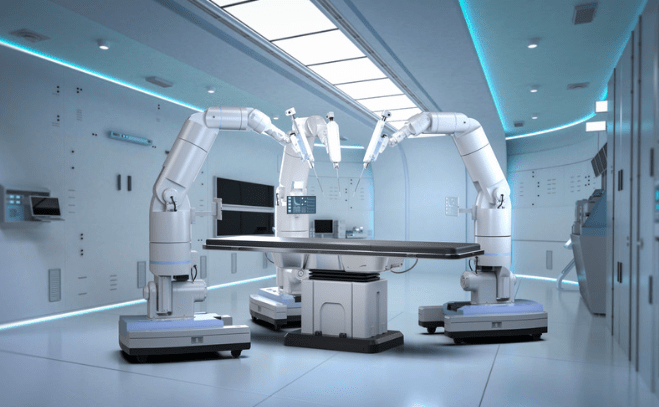
Robotic application is advancing across numerous fields, leveraging the latest developments in AI technology. One notable innovation and increasingly prominent use can be seen in surgical robots.
Traditional surgery is a highly invasive process. To operate, a surgeon must make a large incision to provide access for their hands and instruments to the affected area. Following surgery, patients often face a recovery period that can be lengthy, painful, and uncomfortable.
To address these issues, surgeons introduced laparoscopic surgery, which requires only small incisions to insert thin tubes equipped with specialized instruments and a camera. This significant technique has reduced recovery times and post-operative pain compared to traditional surgery.
Since then, further advancements have led to the development of surgical robots, enabling remote surgeries that can even be performed across continents. These robots are increasingly precise and less invasive, revolutionizing the way surgical procedures are conducted and enhancing patient outcomes.
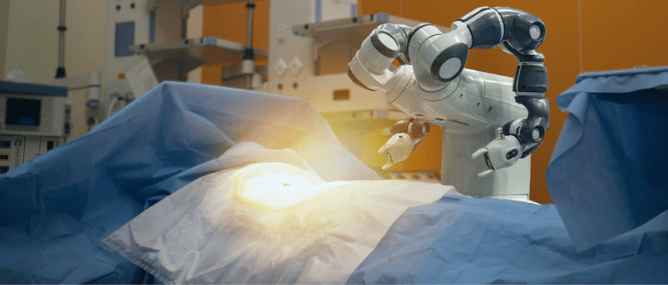
Robotic application in surgery represents a significant advancement in the field of medicine. It requires only small incisions, allowing for minimally invasive procedures. The key difference lies in the control of the instruments: in robotic surgery, the surgeon maneuvers the instruments through a robotic system, utilizing specialized controls that translate their movements into precise actions within the patient’s body.
The uses of robotics in this context are realizing a sort of synergy between human skill and machine precision. This technology allows for enhanced dexterity and visualization, as surgeons can operate with a 3D high-definition view of the surgical site. Additionally, robotic systems can filter out hand tremors, providing a steadier hand than that of a human surgeon.
Moreover, robotic surgery has expanded the range of procedures that can be performed minimally invasively, including complex operations in urology, gynecology, and cardiothoracic surgery. As a result, patients benefit from shorter recovery times, reduced post-operative pain, and lower risks of complications.
The integration of robotics into surgical practices not only enhances the capabilities of surgeons but also significantly improves patient outcomes, marking a transformative shift in modern medicine.
The first surgical robot to receive FDA approval was the Da Vinci System, developed by Intuitive Surgical, in 2000. Since its introduction, Intuitive Surgical has established itself as a leader in the industry, with more than 7,500 Da Vinci robots currently in operation around the globe. Remarkably, a surgeon initiates a procedure using one of these robots every 17 seconds somewhere in the world.
According to a recent report, the market for surgical robots is projected to reach a staggering $11.76 billion by 2029. This forecast highlights the expanding sector and underscores the significant potential of robotic applications in modern medicine, reflecting a multi-billion dollar industry poised for continued growth.
Advanced robotic applications are transforming joint-replacement surgery by enhancing precision, reducing invasiveness, and improving safety. Initially focused on total knee arthroplasty, these technologies are expanding to other joints like the shoulder, ankle, and hip.
These robots perform functions such as contactless bone localization and collaboration with surgeons to facilitate joint replacement procedures. Equipped with advanced “eyes” using cutting-edge computer vision, they accurately assess the position and orientation of a patient’s anatomy, eliminating the need for invasive rods and optical trackers.
Surgeons can use tools like sagittal saws alongside the robotic arm, with the “eyes” providing haptic feedback to ensure precision. Additionally, these robots collect real-time data to refine surgical procedures further.
Clinical studies have demonstrated the effectiveness of bone-localization technology, achieving high levels of precision. Ongoing research aims to make these robots widely available, establishing them as essential tools in the global medical community. Furthermore, the integration of 3D printing in orthopedic surgery is enhancing customization and precision, offering new possibilities for patient-specific implants and surgical planning.
Robotic surgeons are paving the way for the possibility of performing remote surgeries. The first truly complete remote surgery took place on September 7, 2001, when a surgeon in France operated on a patient in New York, a distance of 6,230 kilometers across the Atlantic Ocean. While remote surgeries are feasible, the primary challenge hindering their widespread adoption is network speed. These procedures require ultra-fast networks with minimal latency. As network technology continues to improve, the likelihood of remote surgeries becoming a common practice increases.
Additionally, remote surgeries could enable operations to be performed in space. A surgeon on Earth could control a robotic system that translates their movements to a patient in orbit. Although this concept is still in the early stages, NASA is actively exploring the potential of robotic surgeons in space through MIRA, a small surgical robot developed by researchers at the University of Nebraska-Lincoln.
Currently, none of the available surgical robots are fully autonomous. Systems like the Da Vinci are always under the direct control of human surgeons. While some medical robots, such as the CyberKnife—designed for radiotherapy—exhibit a degree of autonomy, they still require human oversight.
The challenge of enabling a robot to autonomously perform complex surgical tasks is significant for AI researchers and robotics engineers. It is more likely that simpler aspects of surgical procedures, such as wound closure, will be automated first, allowing surgeons to concentrate on the more intricate elements of the operation.
Nevertheless, several research projects are advancing the vision of completely autonomous surgical robots, which is increasingly seen as the “medicina del futuro” in Italy. One notable example is STAR, a surgical robot developed at Johns Hopkins University (JHU), which has successfully conducted near-autonomous surgery on a pig. The term “near” is used because STAR still requires some assistance from a human operator. According to the JHU team, a fully autonomous version of STAR is likely decades away, but they remain optimistic that advancements in technology will enable the first clinical tests on humans within the next five years. This progress highlights the potential of robotic application in transforming the landscape of surgical procedures.
Surgical robots offer numerous benefits, including smaller incisions, faster recovery times, and reduced post-operative pain. Human surgeons also gain advantages, as these systems make operations less physically demanding and provide instruments that are more precise and easier to handle. Enhanced visualization tools allow professionals to access a wealth of information during procedures, improving overall surgical outcomes.
However, the adoption of these robots comes with its own set of challenges. One of the primary obstacles is cost; purchasing and maintaining a surgical robot can run into the millions, making them inaccessible for many hospitals.
Nonetheless, the future of surgery will increasingly involve robotic systems, and the integration of artificial intelligence for robotics will undoubtedly lead to new developments. As technology continues to evolve, we can expect to see a growing presence of surgical robots in operating rooms, transforming the landscape of modern medicine.
Per maggiori informazioni sulla STH e i suoi servizi o per possibili collaborazioni, il nostro team è a tua disposizione.
Compila il modulo o inviaci una mail per discutere di come possiamo lavorare insieme.
